Planning an overseas trip while pregnant? While travel can be exciting, pregnancy introduces unique health considerations that require careful planning and precautionary measures. Understanding the risks and taking proactive steps will help ensure a safe journey for both you and your baby.
Risks to Consider
Infectious Diseases
Pregnant women are more vulnerable to infections, and some can pose serious risks to fetal development.
- Zika Virus – Spread by mosquitoes, this virus can cause severe birth defects, including microcephaly (underdevelopment of the baby’s brain). Learn more.
- Malaria – Pregnancy increases the risk of severe malaria, which can lead to maternal complications and neonatal death. Read more.
- Listeria & Toxoplasmosis – These infections, often contracted through contaminated food, increase the risk of miscarriage, stillbirth, and birth defects.
- COVID-19 & Influenza – Pregnant women are at higher risk of severe illness and complications from respiratory infections.

Higher Risk of Mosquito Bites
Pregnancy increases body temperature and carbon dioxide output, making mosquito bites more likely. This elevates the risk of mosquito-borne diseases such as Zika, Malaria, and Dengue Fever.
Vaccination Restrictions
Certain vaccines and medications aren’t recommended during pregnancy, limiting protection options:
- Live vaccines (e.g., Yellow Fever, MMR, and Chickenpox) are generally avoided.
- Some anti-malarial drugs may not be safe.
Blood Clots (Deep Vein Thrombosis - DVT)
- Pregnancy naturally increases clotting factors, making long flights a risk for blood clots. If a clot reaches the lungs, it can be life-threatening.
Airline & Altitude Restrictions
- Many airlines restrict travel beyond 28-36 weeks due to medical risks.
- High-altitude destinations (over 2,500m) can reduce oxygen levels, affecting fetal development.
Before You Travel: Essential Precautions
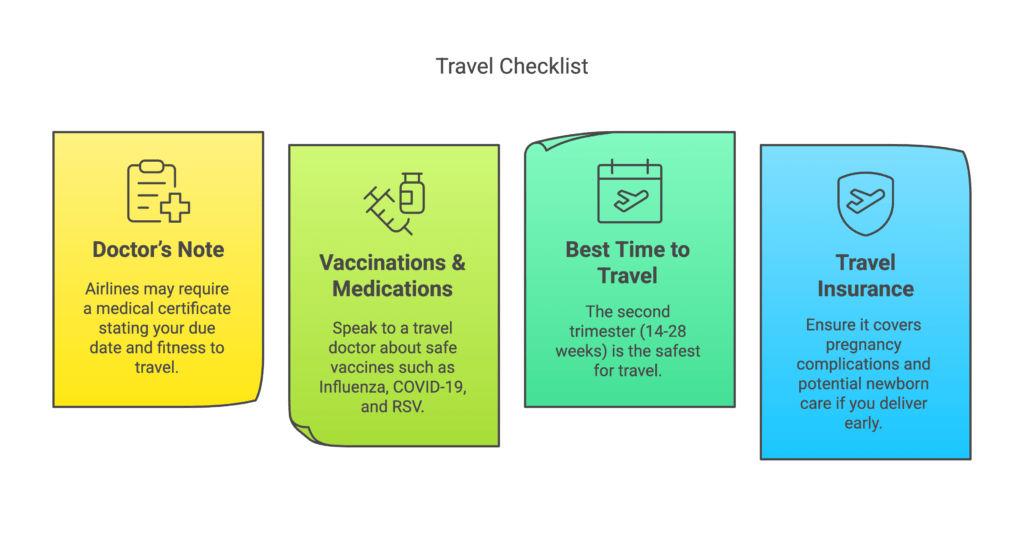
Consult Your Doctor
Before traveling, consult your doctor to obtain medical clearance and confirm that your pregnancy is low-risk. If you have conditions such as preeclampsia, gestational diabetes, a history of preterm labor, or other complications, travel may not be advisable.
Choose a Safe Destination
When selecting a destination, avoid regions with poor sanitation, unsafe water, or high rates of infectious diseases. Additionally, research local medical facilities to ensure that adequate emergency care is available.
Plan for Emergencies
It is also essential to plan for emergencies by having a backup medical care plan in place. Carry a list of emergency contacts and preferred hospitals at your destination to ensure you are prepared for any unexpected situations.
How to Stay Healthy While Travelling
Food & Water Safety
- Avoid buffets, raw seafood, and soft cheeses (high risk for Listeria).
- Drink bottled water only and avoid ice in drinks.
- Do not use iodine to purify water—it can affect fetal thyroid development.

Mosquito Protection
- Use pregnancy-safe insect repellent (≤25% DEET, picaridin, or oil of lemon eucalyptus).
- Apply repellent to clothing instead of skin to reduce absorption.
- Wear long-sleeved, light-colored clothing.
Prevent Blood Clots
- Wear compression stockings on flights.
- Move every 1-2 hours and stretch your legs.
- Stay hydrated.
Reduce Infection Risks
- Wear a mask in crowded areas.
- Wash hands frequently and use hand sanitiser.
Travelling while pregnant requires extra planning to minimise risks. Consult an expert travel doctor before your trip to get personalised advice, safe vaccinations, and expert recommendations.
Book an appointment with your nearest TMA travel doctor today.